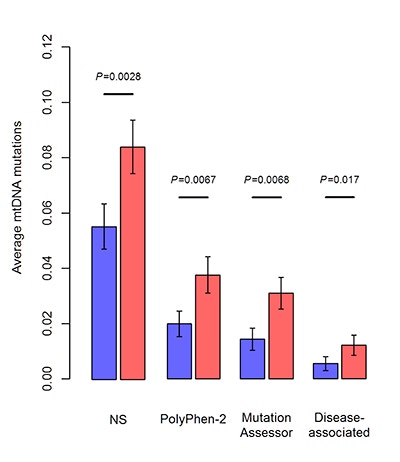
Mitochondria are cytoplasmic organelles that serve a key role in cellular respiration, generating cellular energy and regulating cellular metabolites. Mitochondrial dysfunction has been associated with a variety of disorders, including autism spectrum disorder (ASD), though the underlying cause of this link has remained unclear. Mitochondria contain their own DNA (mtDNA) inherited from the mother, and mutations in mtDNA can lead to mitochondrial dysfunction. As thousands of copies of mtDNA exist per cell, mutations in mtDNA can coexist with copies of wild-type mtDNA within the same cell, a situation referred to as heteroplasmy. Zhenglong Gu and his colleagues evaluated mtDNA heteroplasmy using whole-exome sequencing data from 903 children with autism along with their unaffected siblings and mothers, collected as part of the Simons Simplex Collection. The researchers found that, while children with ASD and their unaffected siblings show similar rates of mtDNA heteroplasmy, children with ASD are more likely to carry predicted pathogenic mutations. Further, children showing higher numbers of predicted pathogenic mutations are more likely to present with intellectual disability. Taken together, these findings suggest that pathogenic mtDNA mutations may contribute to ASD. Further studies of ASD families with mtDNA-targeted deep sequencing and functional assays are warranted.
Reference(s)
Genetic evidence for elevated pathogenicity of mitochondrial DNA heteroplasmy in autism spectrum disorder.
Wang Y., Picard M., Gu Z.