Growth factor improves autism symptoms in mice
Mice lacking a copy of SHANK3, a gene associated with autism and intellectual disability, show marked improvements in brain signaling after being treated with insulin-like growth factor 1, according to unpublished findings presented Saturday at the International Congress of Human Genetics in Montreal, Canada.
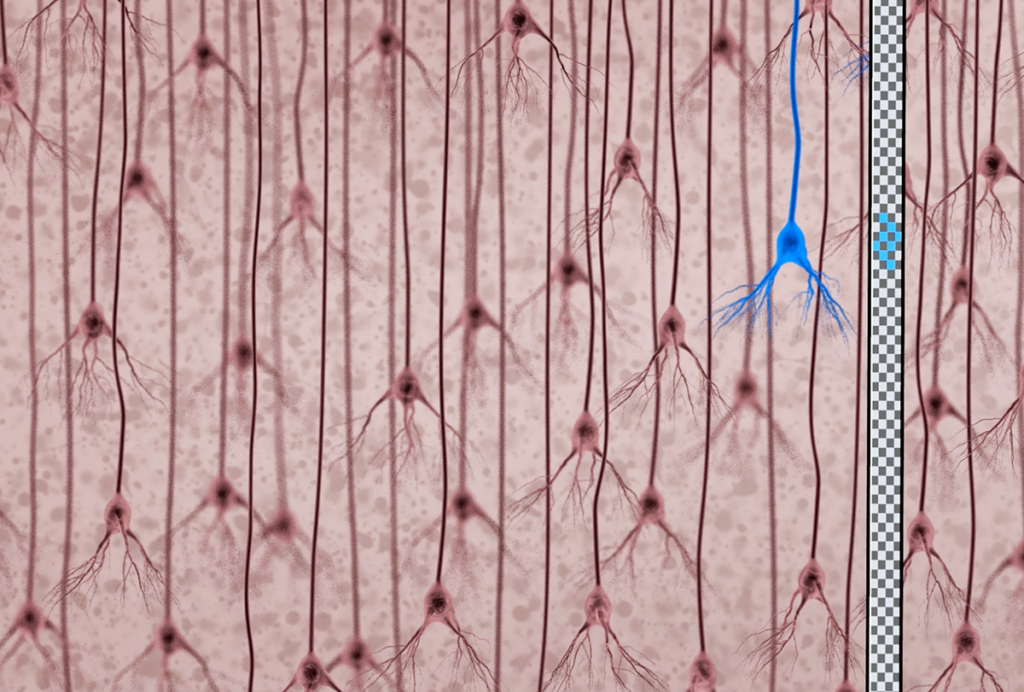
- Growth spurt: Insulin-like growth factor 1, a protein that regulates nerve cell growth and development, shows promise as an autism treatment.
Mice lacking a copy of SHANK3, a gene associated with autism and intellectual disability, show marked improvements in brain signaling after being treated with insulin-like growth factor-1 (IGF-1), according to unpublished findings presented Saturday at the International Congress of Human Genetics in Montreal, Canada.
Impaired expression of SHANK3 prevents synapses, the junctions between neurons, from forming properly. This leads to a defect in signaling between neurons. IGF-1 appears to correct these deficits, allowing nerve cells to communicate normally, says Joseph Buxbaum, who presented the findings at the meeting.
“The synapse is immature in these mice,” he says. “IGF-1 appears to drive the process forward and they become fully mature synapses.”
Based on these findings, the researchers are poised to begin a clinical trial of the drug in children with autism early next year, he says. Because IGF-1 is already approved in the United States for use in children with short stature, the U.S. Food and Drug Administration is allowing the researchers to proceed directly to clinical trials for its use as an autism treatment.
IGF-1 also reverses symptoms of Rett syndrome, a disorder that includes features of autism, in mice1. “We showed that IGF-1 regulates many different signals that can affect synaptic function,” says Mriganka Sur, professor of neuroscience at the Massachusetts Institute of Technology, whose mouse work led to trials of IGF-1 for Rett.
When administered systemically, IGF-1 crosses the blood-brain barrier, which is unusual for such a large molecule, Sur says. Once in the brain, the molecule appears to influence the growth of synapses.
In a safety and efficacy trial of the drug in 12 girls with the disorder, aged 2 to 12 years, a team led by Omar Khwaja at Children’s Hospital Boston has found that the drug does not seem to have anyserious adverse effects.
What’s more, after two weeks of treatment, the drug appears to improve breathing and heart rate, which are abnormal in children with Rett, according to Khwaja, director of the Rett syndrome program at Children’s Hospital Boston.
“The findings are definitely promising,” says Khwaja. “We believe IGF-1 affects a fundamental deficit in autism — abnormal maturation of synapses.”
The researchers are recruiting another 30 participants for a study, set to begin in January 2012, that will fully explore treatment effects.
Amped up:
SHANK3 is located in the chromosomal region 22q13. Deletions in this region lead to Phelan-McDermid syndrome, characterized by extreme intellectual disability, delayed or absent speech, and gait and motor problems. About 80 percent of those with the syndrome also show features of autism.
Buxbaum’s team debuted the first SHANK3 mouse model in December 20102. Since then, two other groups have also introduced SHANK3 mouse models, although each model shows a different set of deficits in social behavior3,4.
SHANK3 is part of the post-synaptic density, a protein complex that helps organize synapses. Two other proteins in the same family, SHANK1 and SHANK2, are also involved in forming synapses.
Evidence suggests that SHANK2 and SHANK3 lay the groundwork for synaptic development, Buxbaum says. “Once they pass a certain threshold, SHANK1 comes in and locks down the synapse,” he says.
In mice that don’t make enough SHANK3, neuronal signaling is disrupted. Specifically, it affects proteins called AMPA receptors, which use the chemical messenger glutamate to create excitatory signals in the brain. “When you knock out one copy [of SHANK3], AMPA receptors do not cluster in the postsynaptic density,” says Buxbaum. Without AMPA, the synapse cannot create the kinds of robust connections between neurons that underlie learning and memory.
Electrophysiological studies of brain slices in the SHANK3 mutants show that IGF-1 turns this around. “If you give IGF-1 to the mice for two weeks, at the clinical dose, you get complete recovery and reversal of these deficits,” says Buxbaum.
The researchers are planning to evaluate IGF-1’s effects in 30 children with Phelan-McDermid syndrome, looking for improvement in core symptoms of autism.
Buxbaum’s group also plans to use quantitative measures to assess IGF-1’s effect on two of the core features of Phelan-McDermid syndrome — motor and severe language deficits. For example, LENA, a digital language processor, detects distinctive speech patterns and can measure improvements in speech.
Children with the disorder also have a distinctive gait, says Alexander Kolevzon, clinical director of the Seaver Autism Center in New York City and an investigator on the study.
“All of these kids have some gait disturbances, delays in achieving motor milestones, low muscle tone. It’s not a typical gait that you would see in someone with other disorders, and it has real functional relevance,” he says.
The researchers plan to use a three-dimensional motion capture system that uses sensors attached to joints to assess improvements in gait.
Sur points out that though hundreds of genes are involved in autism, most affect synaptic function in some way. Testing a drug that is already approved for use in children and has been shown to affect synaptic function in mouse models is, he says, “a rational way of approaching autism therapeutics in a short time frame.”
References:
1: Tropea D. et al. Proc. Natl. Acad. Sci. USA 106, 2029-2034 (2009) PubMed
2: Bozdagi O. et al. Mol. Autism 1, 15 (2010) PubMed
3: Bangash M.A. et al. Cell 145, 758-772 (2011) PubMed
4: Peça J. et al. Nature 472, 437-442 (2011) PubMed
Recommended reading

Expediting clinical trials for profound autism: Q&A with Matthew State

Too much or too little brain synchrony may underlie autism subtypes
Explore more from The Transmitter

Mitochondrial ‘landscape’ shifts across human brain